Respiratory function tests (RFTs), also known as lung function tests are performed so that you and your doctor can understand how well your lungs are working. These tests are essential in the diagnosis of suspected lung disease and in monitoring your response to treatment.
There are a few components of the test, each determining different characteristics of your lung’s health. The three most commonly performed tests are spirometry, lung volumes and gabs diffusion.
Spirometry
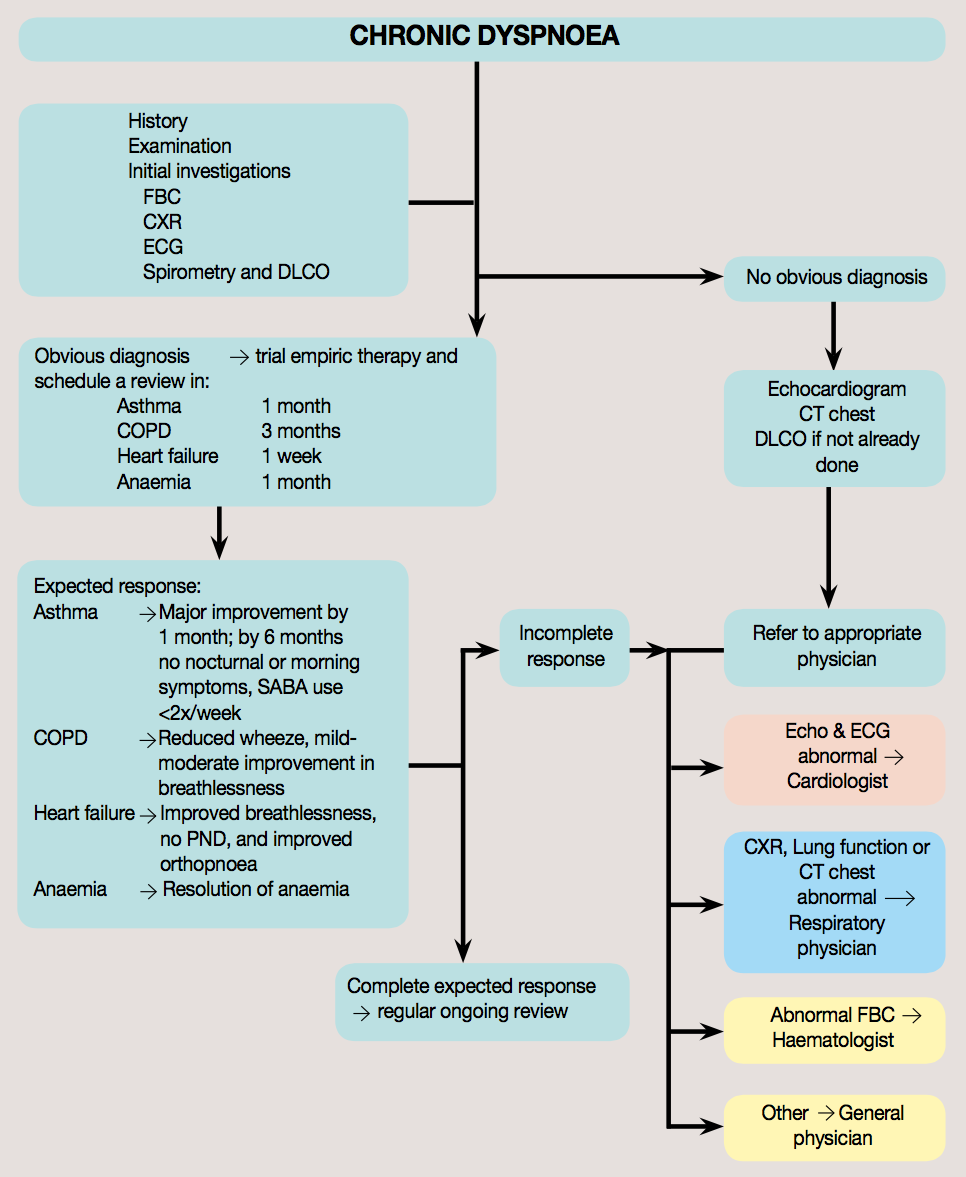
This test requires you to blow out through a mouth-piece hard and fast. It is essential in the diagnosis of chronic obstructive pulmonary disease (COPD) and asthma. To get accurate results, the test is usually repeated at least 3 times with a rest between each blow. This test is then often repeated after a dose of salbutamol (Ventolin) puffer to see if there is any difference.
Lung volumes
This involves getting into our clear glass box called “The body box”. It is like a clear telephone box and the door is shut only a short time while you perform some special breathing techniques with your scientist next to you. If you have trouble with claustrophobia please talk to your scientist prior to the test.
Gas diffusion
This test involves taking some deep breaths of a special gas mixture with a few breath holds. It is quick and easy to do, but you need to avoid smoking prior to the test because this interferes with the test results.
Other important respiratory tests that your doctor may request are
- Bronchial provocation test
- Cardiopulmonary exercise test
- Skin prick testing
- Shunt study
- High Altitude Simulation Test
Blog posts on these tests will follow, so check back soon!
Depending on what tests your doctor performs, the respiratory function tests will take between 30-45 minutes and will be at all times supervised by a Respiratory Scientist.
What are normal results for lung function tests?
Laboratories are able to compare your results from huge data sets of health normal people from all around the world, of all ages, heights, weights, ethnic background and gender. So your results will be compared with the normal standard data of people matched for your height, weight, age, gender and ethnicity. Your own lung function can be tracked over time to help see if you have had a change.
What should I do to get the best results?
- Do not smoke for at least 1 hour before the test.
- Do not drink alcohol for at least 4 hours before the test.
- Do not exercise heavily for at least 30 minutes before the test.
- Do not wear tight clothing that makes it difficult for you to take a deep breath.
- Do not eat a large meal within 2 hours before the test.
What medications should I stop before the test?